Author 1 Name: Yahia Hejazi, M.D, FPICS
Mentor's Name: Younes Boudjemline, M.D, PhD
Editors Name Ziyad M. Hijazi, M.D, FACC, MSCAI, FAHA, FPICS
How I do it: Tips, Tricks, and Techniques
A PICS Society education series
Sinus Venosus Defect Closure
Introduction:
Transcatheter repair of sinus venosus atrial septal defect (SVASD) has become an alternative option to open heart surgical repair. Different operators use different techniques to implant a covered stent in the Superior Vena Cava (SVC) to close the SVASD and to redirect flow of the anomalous vein back to the left atrium. The results of the procedure are good, however, there are potential significant complications related to stent stability in the SVC and potential migration of the stent that need to be addressed. Therefore, the technique is still evolving.
Anticipated challenges of the procedure:
- Patient size: SVC needs to accommodate large adult size stent. Also, the procedure requires relatively large neck and femoral sheaths.
- Availability of long stents to have enough length to anchor SVC and extend to SVC-RA junction closing the Atrial Septal Defect (ASD).
- The foreshortening of about 30-35% for large diameter stents makes stent positioning extremely challenging to predict. (1)
TIP 1. Planning and Preparation
- Access
- RIJV (right internal jugular vein)
- RFV (right femoral vein) and LFV (left femoral vein)
- Imaging
- Cross sectional CT or MRI to measure the SVC diameter, number of anomalous pulmonary veins, site of anomalous drainage (high SVC, SVC-RA junction) and Qp:Qs (Figure 1)
- Other
- 3D printed models (Figure 2)
Tip 2. Tools needed
- Sheaths
- Catheters
- Devices
- Others
Tip 3. How I do it
Details of the technique:
The following technique was developed by Younes Boudjemline, MD. The covered stent was prepared ex vivo as followed: a surgical suture (MERSILK Ethicon KS-75, straight needle, 100-cm long, size 0) was inserted through one of the stent struts (Figure 3). The selected strut was one free of PTFE coverage attachment. The suture was adjusted so that two equal lengths could be held by a needle holder after cutting the needle. The suture itself looped freely around the strut of the stent without a knot (Figure 4).
The stiff guidewire is used to create a rail extending from the femoral vein access and exteriorized from the internal jugular vein. A vascular balloon (12mm*6 cm, Mustang, Boston Scientific, Boston, USA) was then inserted from the RFV over the wire rail and exteriorized through the RIJV sheath [16 Fr Cook or 14-Fr DrySeal based on the availability-as mentioned above, we prefer the DrySeal sheath]. This balloon must be smaller than the SVC diameter and with a shaft long enough to be exteriorized. The chosen covered stent, which is now held by the suture, is crimped over the balloon or its shaft taking care to position the stent with the suture at the SVC side of the stent. The stent-balloon assembly is advanced from the RIJV to the RA by pushing on the stent and pulling the balloon from the RFV into the RJV sheath. Of note, when a Cook sheath is used, a protective tubing is used to go through the hemostatic valve to avoid damaging the stent cover. In such cases, the protective sleeve is passed over the balloon onto the shaft before mounting the stent, with the conical extremity closest to the balloon. The protective sleeve is then retracted to cover the stent. This is not needed when DrySeal sheath is used. When needed (when the stent is crimped on the shaft), the stent is positioned on the balloon by applying some tension on the suture while pulling on the RFV end of the balloon catheter. The balloon is then inflated to expand the stent in the SVC. While injecting contrast from the RIJV sheath, stent-balloon assembly is positioned in the intended final position. At this stage, the stent is free (i.e., not apposed to the wall) in the SVC and held by the suture (Figure 5). The stent position can be re-adjusted to have enough stent length in the SVC for good anchoring along with caudal end below the inferior rim of the defect to cover the ASD as confirmed by TEE. The small balloon is then removed (while holding the stent in position with the suture) and replaced by a larger balloon (equal to SVC diameter) with the intention to flare the atrial part of the stent (Figure 6). This step is done under TEE guidance (Video 1). After deflation of the balloon, the position of the stent is assessed. If too low, some traction is applied to the suture to pull the stent into the SVC. If too high, the balloon is slightly re-inflated in the SVC stent and the stent-balloon assembly is pulled down to have more stent in the RA. When the position is satisfactory, the SVC stent is finally fully inflated to fully appose the wall and to seal the defect (Video 2). To avoid embolization after suture removal, angiogram in the SVC is repeated at this stage to carefully assess if the stent length is long enough in the SVC for adequate anchorage. If the length is deemed inadequate, an overlapping BMS could be positioned while still holding the covered stent with the suture. Otherwise, no additional stent needs to be placed. Importantly, the suture is removed by inflating a balloon to hold the stent while pulling on one extremity of the suture until complete removal of the suture. The balloon is then deflated, and wire and catheters are removed. The same technique must be used if a BMS is placed to secure covered stent. Antibiotic and heparin prophylaxis is given to patients according to institutional protocol.
Pitfalls to avoid
- Contrary to conventional stent placement where the stent can move from the balloon to the shaft during advancement in the long sheath, here, because the balloon is pulled through the sheath, the stent can slide off the balloon. When crimped on the shaft, a slight balloon inflation facilitates the advancement of the stent–balloon catheter assembly without risk of stent slippage off the balloon. In addition, crimping on the shaft allows to reduce the profile of the stent–balloon assembly by 1-2 Fr (profile of the shaft 5.8-Fr, balloon profile 7-Fr). In practice, we kept the same sheath size but the stent assembly moves more freely.
- Avoid embolization after suture removal: angiogram in the SVC needs to be repeated at this stage to carefully assess if the stent length is long enough in the SVC for adequate anchorage.
- Removal of suture: inflate a balloon to hold the stent while pulling on one extremity of the suture until complete removal of the suture.
Tip 4. What complications to expect and how to deal with them
- Pulmonary venous obstruction: A dedicated catheter (from the LFV) needs to be kept in the right upper pulmonary vein (RUPV) until the end of the procedure to monitor the pressure in this vein. Patency and re-routing of anomalous pulmonary veins to left atrium (LA) are confirmed with venogram and simultaneous pressure monitoring in RUPV and LA with balloon fully inflated in the SVC (Video 3). Use a non-compliant balloon to occlude the SVC. This prevents bulging in the mouth of the anomalous vein that may lead to occlusion of this vein.
- Distal end of the stent crossing the atrial septum resulting in residual shunt: This can happen because of inadequate flaring and inadequate length of stent to cover the inferior margin of the defect. Pushing the stent down would not be possible. If the residual shunt is minimal, nothing should be done. If significant, another covered stent should be implanted overlapping the first stent, but with its inferior margin covering the defect completely. Implantation of the second stent should follow similar steps as above. Alternatively, a device can be implanted in this residual defect to occlude it.
- Embolization: suture technique is considered a very good safety measure to avoid stent embolization. However, interventionist should employ all efforts to prevent this complication. The stent assembly should extend at least to the level of azygos vein. If the SVC portion of the stent is too short, a bare metal stent (BMS) needs to be placed. Moreover, it is only once the desired position of the stent is achieved with good stability that the suture can be released. In a case series from Sidra Medicine, not published yet, no additional stent was needed to secure the covered stent.
Summary:
The suture technique is a novel and safe modification of conventional SVASD exclusion using a covered stent. This technique allows precise positioning of the covered stent with multiple adjustments. In addition, the stent is secured until the removal of the suture, thus giving the operator time to decide if an additional stent in the SVC is required to stabilize the covered stent.
References:
- Rosenthal E, Qureshi SA, Jones M, Butera G, Sivakumar K, Boudjemline Y, Hijazi ZM, Almaskary S, Ponder RD, Salem MM, Walsh K, Kenny D, Hascoet S, Berman DP, Thomson J, Vettukattil JJ, Zahn EM. Correction of sinus venosus atrial septal defects with the 10 zig covered Cheatham-platinum stent - An international registry. Catheter Cardiovasc Interv. 2021 Jul 1;98(1):128-136. doi: 10.1002/ccd.29750. Epub 2021 May 7. PMID: 33909945.
- Hansen JH, Duong P, Jivanji SGM, Jones M, Kabir S, Butera G, Qureshi SA, Rosenthal E. Transcatheter Correction of Superior Sinus Venosus Atrial Septal Defects as an Alternative to Surgical Treatment. J Am Coll Cardiol. 2020 Mar 24;75(11):1266-1278. doi: 10.1016/j.jacc.2019.12.070. PMID: 32192652.
- Selected Abstracts from the PICS Society Symposium 2021 Aria Convention Center Las Vegas, NV September 1–4, 2021. Pediatr Cardiol 42, 1890–1946 (2021).
- Abdullah HAM, Alsalkhi HA, Khalid KA. Transcatheter closure of sinus venosus atrial septal defect with anomalous pulmonary venous drainage: Innovative technique with long-term follow-up. Catheter Cardiovasc Interv. 2020 Mar 1;95(4):743-747. doi: 10.1002/ccd.28364. Epub 2019 Jun 14. PMID: 31197932.
figures:
Figures with legends:
Figure 1
Note the slightly more gradual curve compared to the 5 Fr. RCA
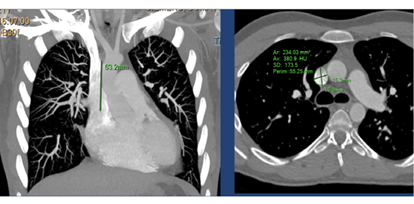
Figure 2
3D printed model: probe inserted in the anomalous pulmonary vein reaches left atrium. B: Stent is placed in SVC-RA junction and the probe in anomalous vein confirms patency of venous drainage while stent in situ.
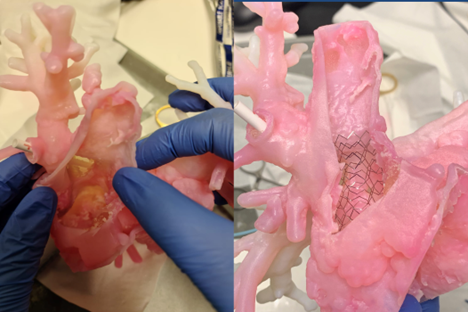
Figure 3
Needle is inserted through one of the SVC stent struts. The selected strut was one free of PTFE coverage attachment. PTFE: Polytetrafluoroethylene

Figure 4
Two equal lengths are held after cutting the needle. The suture itself looped freely around the strut of the stent without a knot
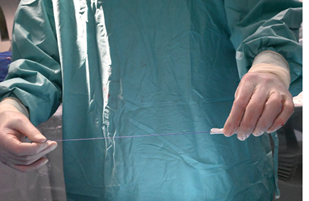
Figure 5
The stent is free in the SVC, and is secured by the suture
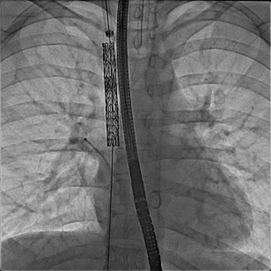
Figure 6
Fluoroscopic still image: AP view, covered stent in SVC excluding anomalous right pulmonary vein and extending to ASD part of the defect. The balloon is inflated to flare up the distal part of the stent to close the ASD. Note a catheter is kept in the anomalous pulmonary vein to continuously measure pressure and check for obstruction during and/or after the balloon is fully inflated.
AP: anteroposterior, ASD: atrial septal defect

Video 1:
TEE, bicaval view at 110 degrees (focusing on SVC, IVC not shown), shows stent in SVC with balloon fully inflated to close the ASD. No residual shunt is seen. TEE: Transesophageal echocardiogram
Video 2:
TEE, bicaval view at 110 degrees (focusing on SVC, IVC not shown), shows stent in SVC with balloon fully inflated to close the ASD. No residual shunt is seen. TEE: Transesophageal echocardiogram
Video 3:
Cine Angiogram (AP view), injection in anomalous pulmonary vein while balloon is fully inflated in SVC confirms patency and re-routing of anomalous pulmonary veins to LA